How to Develop Pharmacy Management Software: Authoritative Guide

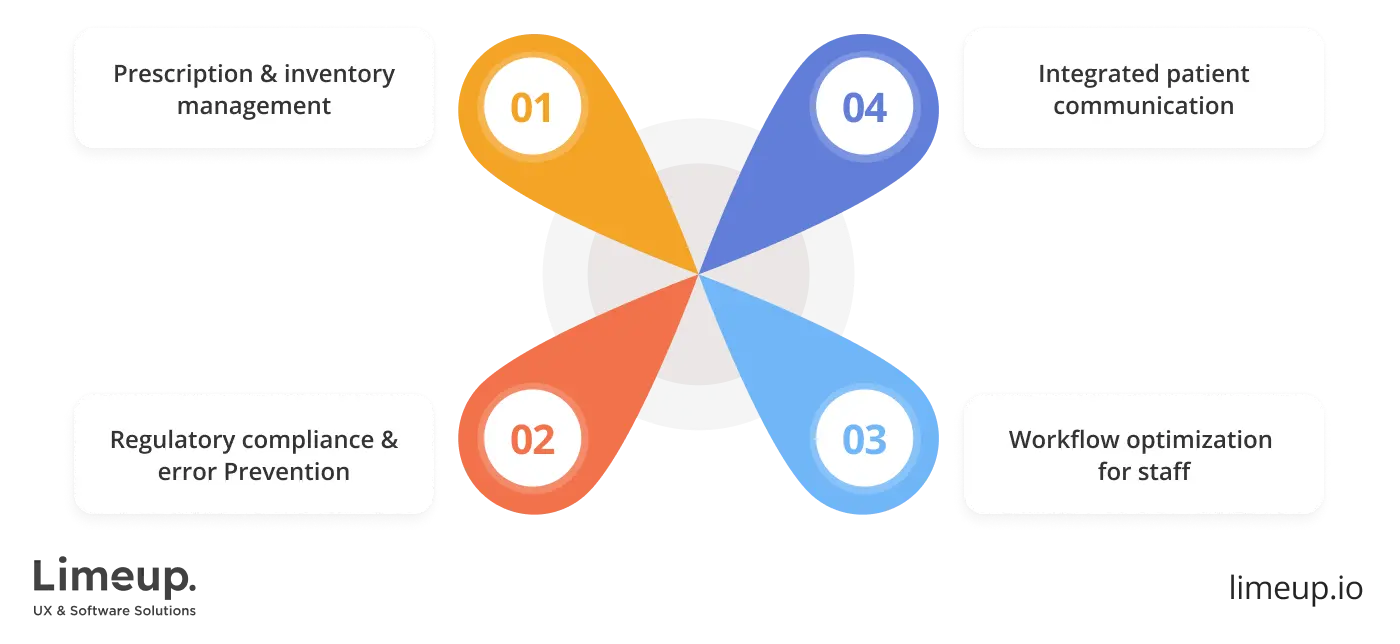
Pharmacy management software development is no longer a back-office concern as it’s at the heart of efficient wellness services. As prescription volumes grow and regulations tighten, pharmacies need more than spreadsheets and paper trails to keep up. This overview offers a practical summary for flipping the switch to digital, covering everything from system architecture to the real-world demands of the healthcare sector.
When you set out to build pharmacy management software, you create a code that shapes how pharmacies care for communities. Behind every filled prescription is a chain of tasks: inventory checks, dosage validation, compliance steps, and patient records. Designing a system that keeps all that moving smoothly requires both technical clarity and domain insight, a balance we’ve been fine-tuning at Limeup.
Pharmacy management systems today are wired for action—forecasting stock shortages, noticing risks and uncovering valuable findings. In the pharmaceutical world, care doesn’t end with prescriptions, and software keeps it moving safely. After a decade immersed in medical solutions, we know the terrain and we’re here to walk you through it.
What is a pharmacy management system?
Pharmaceutical operation digital tools are the central hubs that support day-to-day operations in medication-focused environments. These tools handle everything from prescription processing and inventory control to payment coordination and regulatory compliance. With smooth operations, they allow drugstores to maintain pace with efficiency, even during peak hours.
The ultimate goal is to develop pharmacy management software that reduces the workload of staff and minimizes human error. If effectively put in place, it detects possible medication conflicts, triggers items that are running low and offers a single interface to check for prescription correctness.
Such kind of workflow establishes credibility between healthcare providers, decreasing the likelihood of fatal errors during medication handling.
Patients, in turn, gain quicker access to treatment and a safer therapeutic experience.
There’s a difference between writing code and solving real problems. Pharmacies face constant demands—tight schedules, strict rules, and zero room for error. Custom healthcare software development responds to these realities by creating tools that reflect how people work, not how software thinks. From compliance to workflow patterns, everything is tailored with care.
No matter the scale, single outlet or national brand, the mission is clear: equip healthcare professionals with tools that lighten their load and elevate patient care. Behind the scenes, specialized software quietly drives daily operations, helping teams spend less time navigating interfaces and more time focused on real interactions.
These digital solutions also open new doors for patient engagement. With built-in communication functions, patients are sent timely reminders about their medication, medicine heads-ups and refill reminders without ever leaving their phone.
Revolutionary interactions of this kind build trust between healthcare professionals and patient populations, building a more loyal and contented customer base. A systematic review published in the Journal of Medical Internet Research found that 88.8% of the studies had a positive influence on patient behavior and 82.9% showed improvement in patient participation through information technology platforms.
How to create a pharmacy management system in 7 steps?
The generation of a dispensary operation solution begins by understanding the complex challenges healthcare providers face daily. In an environment where every decision affects both patient outcomes and business performance, precision is urgent.
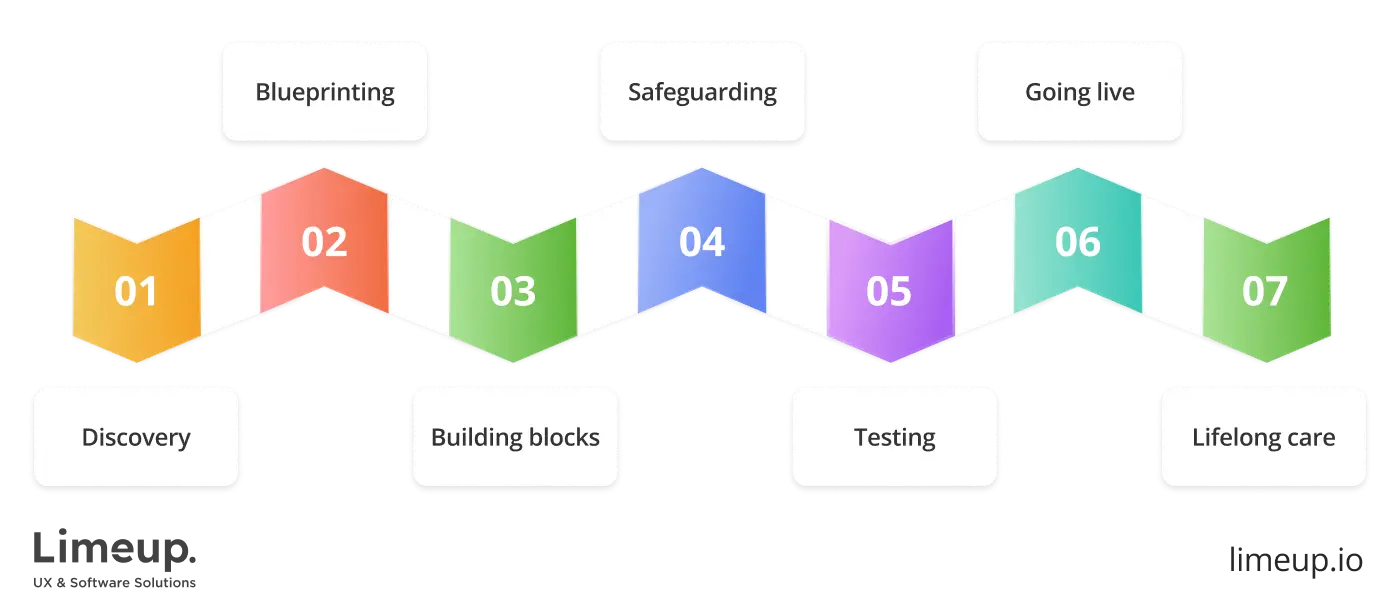
Discovery — stage 1. The foundation of building a pharmacy management system lies in comprehending the workflow of a dispensing operation. Limeup’s coders team up with the staff pharmacists, technicians and supervisors to fully understand the challenges they navigate daily.
Immersing ourselves in the workflow uncovers time drains, inefficient methods and regulatory hurdles that impact day-to-day operations. Only then may the solution be crafted to tackle real issues, improve efficiency and refine processes without skipping a beat.
Blueprinting — stage 2. After the insights have been gathered, the design process starts. The goal is to translate needs into simple and intuitive visual language. Interfaces are crafted in a way to reduce friction and increase efficiency so that pharmacists are able to center on work and not button deciphering. What matters here is structuring the project to meet practical needs, creating end-product that’s intended to be effective and simple to use in day-to-day activities.
Building blocks — stage 3. As the idea transitions into technical phases, programmers are involved in writing code, determining which tools suit the size and needs of the project best. Where there are great numbers of transactions, the back-end is working to keep it in motion without a glitch even under stress.
At the front-end, it’s all about UX, intuitive and flowing. Behind the scenes, managing data means that it’s all there, all making sense, available at short notice, and secure. We’ll unpack the nitty-gritty of how all the pieces fit together soon.
Safeguarding — stage 4. To develop a pharmacy management system with built-in digital protection means placing confidentiality at the heart of the design. Prescription records, dosage levels and patient data all require ironclad security to keep curious eyes away.
It’s a question of adding the right compliance prerequisites and wrapping it all in state-of-the-art encryption methods, keeping sensitive information under lock and key. Permission controls, credential policies and activity monitoring become the behind-the-scenes heroes, built into the system to keep things running smoothly. We’ve got your back at each step of the way, with confidentiality never being compromised.
Testing — stage 5. Validation is a continuous process, like having an eagle eye on all the details. Code ninjas test individual components before stepping back to view the big picture, attesting everything ticks like clockwork. Load testing is like having a party at rush hour, pushing the software to its limits to determine if it will stand the test.
Going live — stage 6. After being thoroughly tested, the solution reaches the launch phase. The shift from staging to production is accomplished cautiously, with data integrity maintained and compatibility with current dispensing tools. Workshops is a top priority and the employees are trained on the platform through interactive sessions so that they are prepared right from day one.
Lifelong care — stage 7. Once the solution goes live, the work continues behind the scenes. Healthcare obligations change and the software must stay current with new guidelines and tools. Updates are released periodically, enhancing functionality and addressing any issues. A strong support system makes dispensing teams never feel in the dark.
Over time, the software comes of age along with the pharmacy it supports. With each update and adjustment, it remains in sync with healthcare’s demands. Built right, it becomes something the staff can rely on without second thought.
What is the tech stack for pharmacy management software development?
Behind every reliable drug inventory tracking solution is a carefully selected technology stack. Each component, front-end, back-end, database, infrastructure, is chosen to guarantee the platform performs efficiently, remains secure and scales effortlessly as demands grow. Within a high-stakes healthcare setting, the goal is to pick solutions that are useful and pragmatic, as opposed to doing what’s popular.
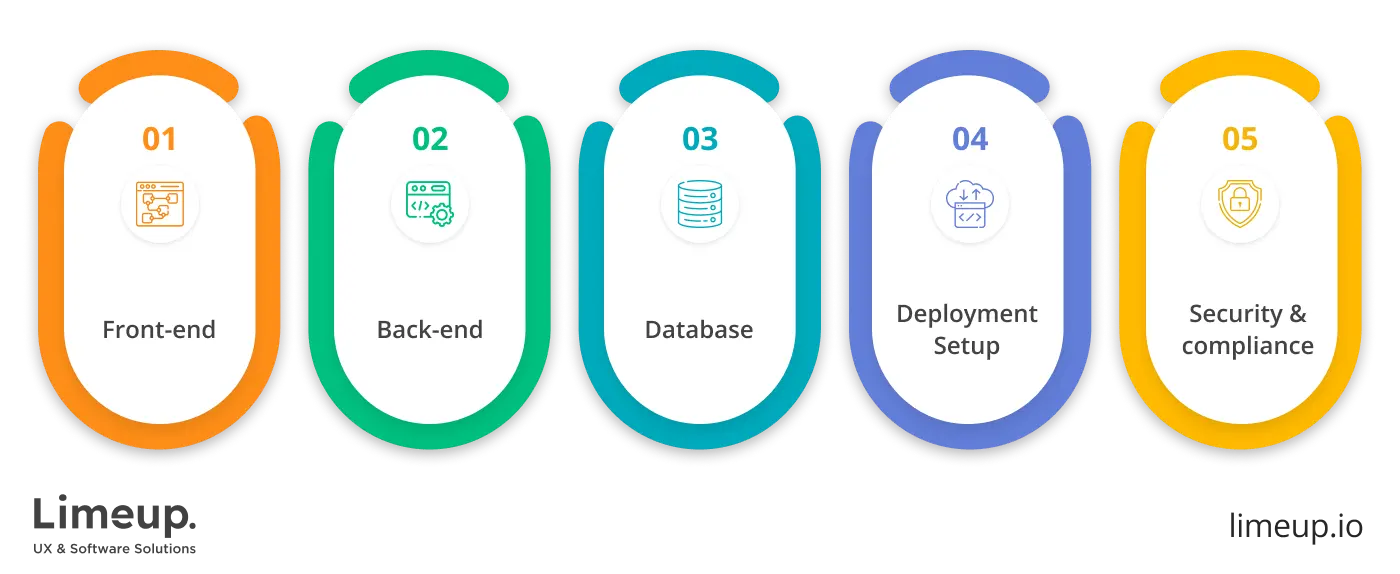
— Front-end
Imagine a dispensing environment where every movement is fluid — a smooth flow with no lag and no confusion. That’s what an instinctively designed user interface can accomplish. Libraries like React.js and Vue.js open up possibilities for digital creators to build dashboards that bring clarity and speed to every aspect of the workflow, freeing staff to focus on whatever matters most.
Such tools present an adaptable framework that responds to the varied tasks and operational patterns inherent in clinical environments. For in-house use with mobile apps or tablets, React Native or Flutter employ cross-platform technology to condense pharmacy management system development time while keeping the experience consistent.
— Back-end
On the server side, the standards are flexibility and performance. Node.js is great at running several processes simultaneously, which is important for handling prescriptions, inventory, and billing. However, Ruby on Rails and Django still fit in because they offer mature environments with strong security features, ideal for running the back-end processes like reminders for dosages, prescription tracking, and reporting of compliance.
— Database
Data flows continuously in every corner of a pharmacy, with patient records, transactions, and medication history needing fast, secure access. PostgreSQL is the best fit for data with structure due to its power and feature-based architecture.
Yet, when flexibility becomes indispensable, such as with varying formats of prescription or supplier data, MongoDB offers the ability to easily adjust. Often, pharmacies combine SQL for structured data and NoSQL for dynamic needs, optimizing both reliability and adaptability.
— Infrastructure and deployment
As for scalability and uptime, nothing beats the reliability of AWS, Google Cloud, or Microsoft Azure. With these cloud services, we ensure that your solution can scale and adapt to growing demands while remaining secure and efficient. Limeup uses these platforms to provide solid, fast deployment and robust system monitoring.
Docker and Kubernetes allow us to package components into containers for efficient deployment and maintenance. This method provides a hassle-free way to implement updates without taking your operations offline. Microservices architecture cultivates steady coding progress with minimal disruption, keeping changes isolated from your ongoing work and boosting flexibility.
— Security and compliance
Handling patient data means the tech stack must incorporate layers of protection. OAuth 2.0 and JWT help with secure authentication. TLS encryption, regular vulnerability scans and real-time monitoring ensure compliance with standards like HIPAA in the US or GDPR in Europe. Logging and alerting tools such as ELK Stack or Datadog provide visibility into every corner of the system, helping catch issues early.
What are the key features of a pharmacy management solution?
Behind the counter, every action is guided by urgency, responsibility, routine that leaves no room for guesswork. When every moment counts, digital solutions need to act with the same urgency. Not by offering everything, but by elevating what matters most: fast access, dependable results and operational clarity.
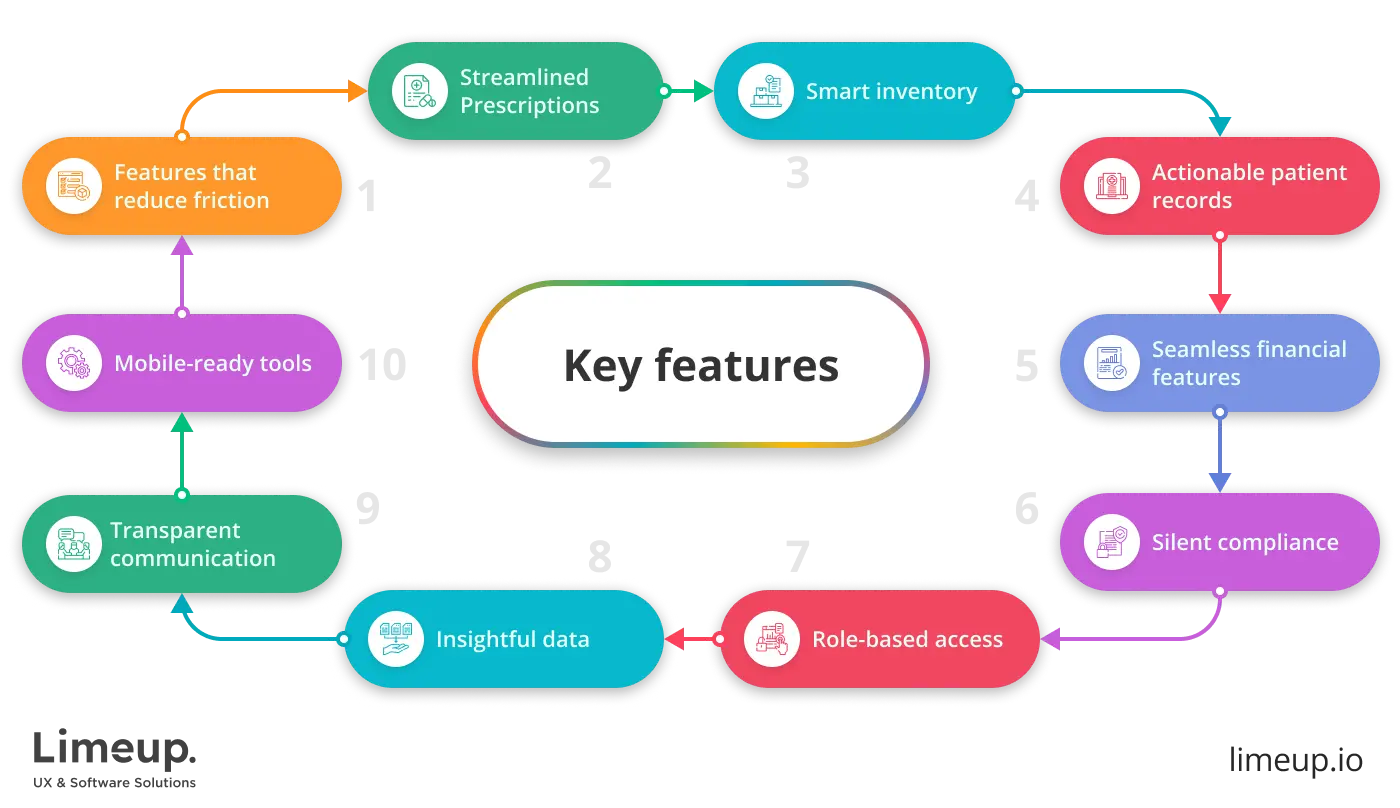
- Systematized prescription handling
Prescription management depends on speed, accuracy and smart coordination. Well-structured workflows catch missing details, highlight concerns and help pharmacy teams move from review to approval with ease. Automated steps like dosage checks and refill alerts trim delays and reduce mistakes.
- Inventory that talks back
Stock control works best when there’s no need to hunt for answers. Clear observations into usage, expiry timelines and order delays allow pharmacies to act fast and avoid running low on essentials. Restocking becomes a rhythm, not a reaction. A well-ordered supply flow means fewer interruptions and more time spent supporting those who need it most.
- Patient records that stay useful
Pharmacy work builds patient stories one prescription at a time. Keeping tabs on medication history, sensitivities and dosage changes should be as intuitive as flipping a page. Automated prompts for refills or missed pickups keep both sides moving forward. Over time, that consistency builds trust.
- Financial features that reduce friction
Processing payments and handling insurance shouldn’t feel like untangling a knot. Uncomplicated billing tools handle transactions smoothly and link with providers to reduce back-and-forth. Clear breakdowns, instant co-pay calculations and quick claim submission keep things moving. That kind of clarity helps avoid frustration at the counter.
- Compliance that works quietly in the background
Rules in healthcare aren’t optional and following them demands precision. Every click, entry and change should be logged automatically, with records locked down tight and ready for audits. Regular updates to policies and clear user trails help teams stay on the safe side. It’s about working smart without walking a compliance tightrope.
- Access that reflects roles
Each role in a pharmacy has distinct access needs. By assigning permissions based on job function, privacy and accountability are safeguarded. Pharmacists have the full scope of patient histories, while front-desk staff see only what’s relevant to their duties. This approach helps rationalize operations and reduces the chance of accidental errors.
- Data that teaches, not just tracks
Built-in analytics let pharmacy managers dig into patterns. What’s selling quickly? Which medications need more shelf space? How are peak hours affecting refill turnaround? Reports based on real numbers give decision-makers tools to adapt their approach with confidence.
- Clear internal and external communication
Pharmacies function as a bridge between medical professionals, patients and insurers. For ease of coordination, secure avenues for real-time information are needed, diminishing necessity of follow-ups or clarifications. Direct messaging and notifications accelerate decision-making by lessening bottlenecks.
- Flexible tools for on-the-move operations
The boundaries of clinical practice have extended. Staff must be in a position to manage stock, process requests and deal with records with equal ease in the back office or when on the move. Cross-device accessibility keeps everything running without a hitch.
Every element is purposefully designed to keep pace with the dynamic demands of the work. A truly effective solution doesn’t disrupt the workflow as it empowers staff, maintaining consistent delivery and the ability to adapt as circumstances evolve.
How much does it cost to build pharmacy management software?
Medicinal distribution services don’t follow a universal playbook. Each one runs with its own rhythm, shaped by local regulations, patient demographics and business goals. Because of this, the investment required to build a medical dispensary management toolset fluctuates.
At the most basic level, a smaller, independent healthcare supply counter might need only central functions: prescription tracking, inventory control, basic patient profiles. Building that kind of lightweight system can start around $30,000–$50,000. Larger systems that support multiple branches, link with external health records and handle advanced analytics quickly push pharmacy management system development costs into six-figure territory.
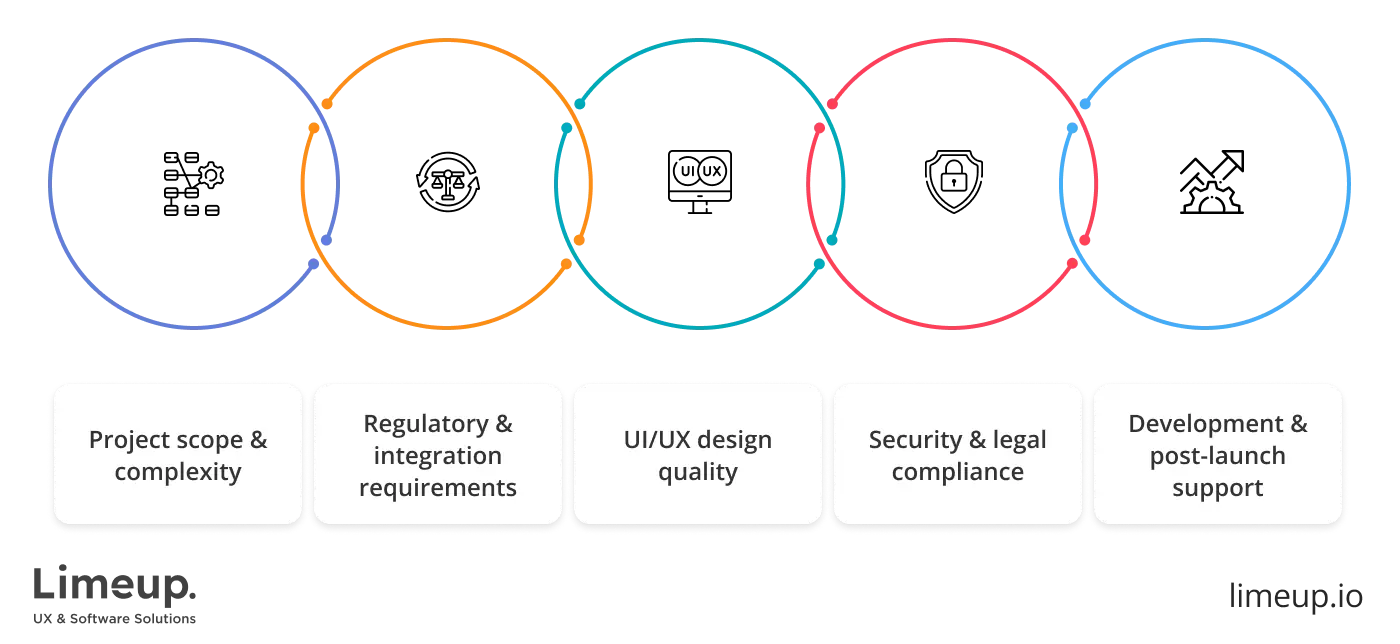
Sophisticated additions like AI-driven demand planning, digital insurance handlers, or barcode tracking call for in-depth customization. Each of these touches multiple points across the workflow and demands real-world validation. Integrating with health authorities or insurer databases demands significant time, along with strict adherence to regulatory responsibilities, all of which impact the final cost.
Interface quality often defines first impressions. In a drugstore operation setting, infrastructures that feel clunky or slow risk being sidelined. Every shortcut, dropdown and color scheme matters when the stakes are high. Dedicated developers often collaborate with specialists trained to design for clinical environments and that level of detail adds to the project’s cost.
Security in pharmaceutical unit software is built on legal requirements, not convenience. Jurisdictions impose different frameworks, but all require features that enforce privacy by layout. Layering in access restrictions, secure storage and logging mechanisms adds creation time. For global deployments, costs often rise due to formal inspections and regulatory certification.
The launch doesn’t mark the end of spending on pharmacy delivery management software development. Behind the scenes, systems must be hosted, maintained and kept current. Subscription-based platforms demand steady investment, while in-house deployments rely on purchased hardware and dedicated staff. Changes in pharmaceutical guidelines or new regulatory directives may trigger frequent software adjustments.
Rates vary depending on where your software pit crew is based. Agencies in the UK or the US may charge noticeably more than their counterparts in Eastern Europe or Southeast Asia, but often offer direct access to local compliance expertise. Working with a team that understands healthcare regulations within your region can reduce risk and save money in the long run.
Programming cost by team type
| Type of developer | Estimated hourly rate | Pros | Cons |
| Freelancers | $25 – $70 | Budget-friendly, flexible availability | May lack deep expertise, limited support |
| Small local agency | $50 – $100 | Easy communication, personalized approach | Slower delivery, fewer resources |
| Mid-sized engineering firm | $80 – $150 | Balanced expertise, project management included | Higher cost, may juggle multiple clients |
| Enterprise-level agency | $120 – $250+ | Full-stack capabilities, precision-driven QA and standards-compliant workflows | Premium pricing, less flexibility |
| Offshore development team | $20 – $60 | Lower rates, round-the-clock work cycles | Time zone gaps, quality can vary |
| In-house team | Varies ($100k+ annually) | Dedicated focus, complete control | High overhead, recruitment and training required |
How to choose a pharmacy management software development company?
Creating digital tools for a medical dispensary isn’t something you hand off lightly. You’re putting the backbone of your clinical operations in someone else’s hands and that level of trust needs to be earned. The following questions are crafted to spotlight teams who can deliver exactly what your healthcare outlet requires—no vague promises, no guesswork.
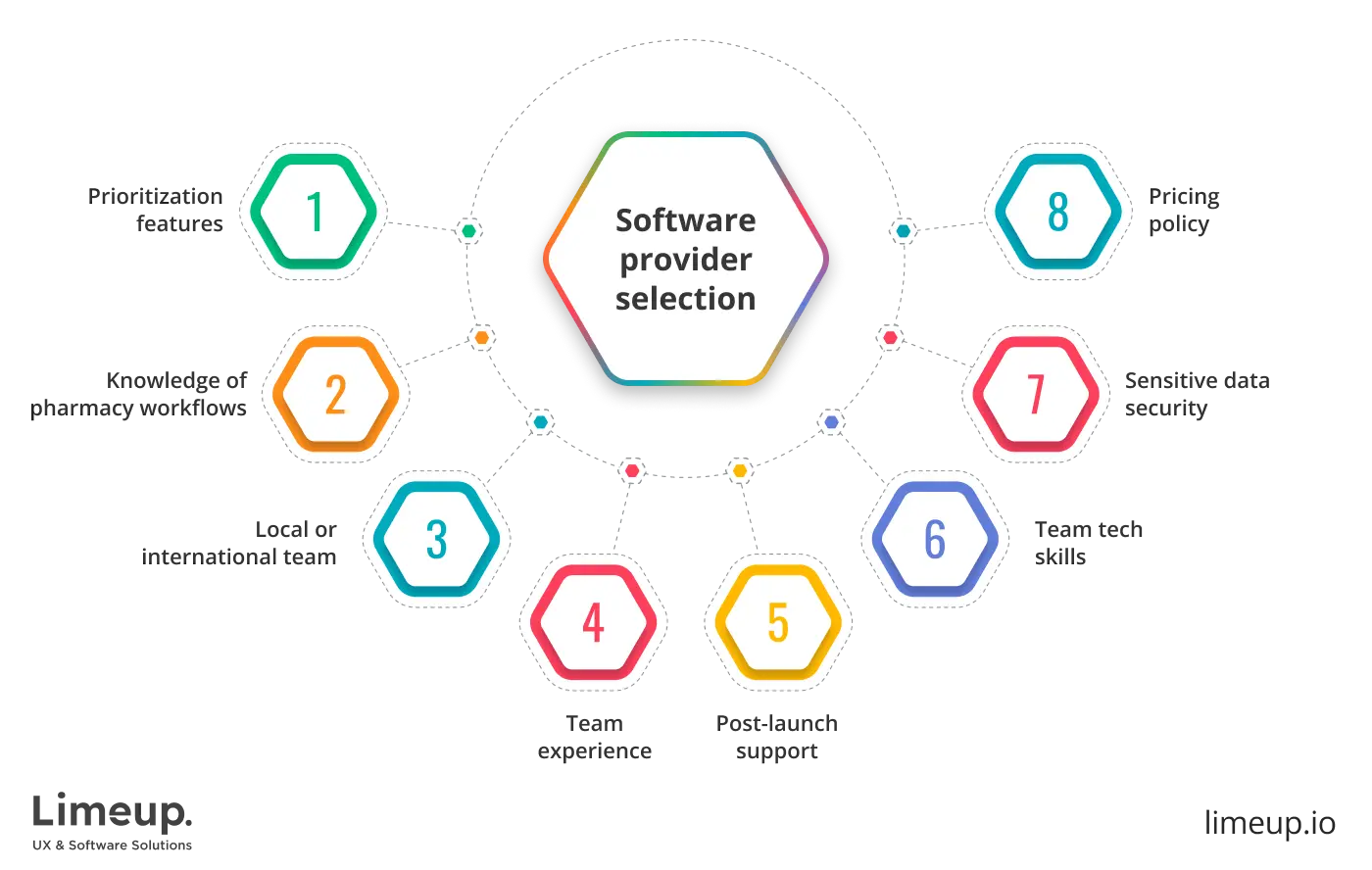
What should I prioritize when evaluating a development partner?
Start with their industry familiarity. A generalist agency might know how to build pharmacy management software, but dispensing environments come with their own rules, routines and regulatory demands. Look for a team that understands code, the daily realities of dispensing, inventory, insurance claims and data privacy.
How can I tell if they truly understand pharmacy workflows?
Ask detailed questions. Can they take me through how prescription processing, batch recall, or multi-store coordination works? Do they have suggestions on how to accelerate tasks or reduce error rates? A reliable partner won’t nod in affirmation—they’ll challenge assumptions and suggest smarter paths.
Should I work with a local team or go international?
Location matters, but it’s not the only factor. A local custom Healthcare software development company might offer on-site assistance, but a global partner might have experience with several healthcare systems. Focus on proven communication processes, time zone coverage and their ability to adapt to your operational hours.
What kind of experience should they have?
Not every successful tech agency is equipped for clinical supply hub projects. Prioritize firms with healthcare case studies or pharmaceutical clients in their portfolio. Limeup, for example, shines with a history of crafting bespoke solutions specifically for the healthcare industry. Bonus points if they’ve worked with regulatory frameworks like HIPAA, GDPR, or MHRA.
How important is post-launch support?
Vital. To create pharmacy management software, a well-built system today may need tweaks tomorrow—medication databases change, regulations flourish and staff feedback surfaces new needs. Your partner should offer long-term collaboration, not a one-and-done drop-off. Ask about their update cycles, SLA terms and escalation processes.
What technical skills should I expect from them?
They should be fluent in modern tech stacks—frameworks like React or Angular for the frontend, well-established back-ends like Node.js or Django and secure, scalable databases like PostgreSQL or MongoDB. But just as important is how they handle integrations, with POS systems, insurance APIs, or e-prescription platforms.
Can I trust them with sensitive data?
Only if they treat security as a first-class priority. Encryption, access logs, authentication layers and regular audits should be standard. Don’t settle for vague assurances—ask how they handle breaches, what their encryption methods are and how often security reviews occur.
How do I assess their coding process?
Transparency is key. Ask how they run sprints, involve clients in feedback loops, and track bugs. A professional team will have a structured, visible workflow. If you’re kept in the dark during programming, you’ll be flying blind when it goes live.
What’s a red flag to watch out for?
Overpromising. If they guarantee full delivery in record time, without gathering detailed requirements or conducting a discovery phase, be wary. A reliable firm will insist on understanding your needs before estimating timelines or quoting costs.
Should price be a deciding factor?
It matters but only in context. A lower bid might come at the expense of maintainability, security, or user experience. Instead of aiming for the cheapest option, look at value. A well-built system that needs fewer fixes and adapts well over time will cost less in the long run.
Why build your medical store management software with Limeup?
Pharmacy handling software is no longer a quiet player in the back office—it’s now a central cog in the healthcare machine. As prescription volumes rise and regulations grow more complex, cyber transformation becomes fundamental for staying afloat. This synopsis offers a real-world breakdown of what it takes to go digital, from architecture to deployment, for anyone looking to build a future-proof system.
Building pharmacy management software is as much about enabling care as it is about developing software. Behind every prescription is a string of coordinated steps: inventory checks, dosage verification, patient record updates and compliance workflows.
A platform that unifies all functions relies on technical proficiency and an appreciation for the specific demands of pharmacy work. That’s the kind of balance Limeup has been honing through years in healthcare tech.
Today’s pharmacy systems are wired to think ahead. They forecast inventory shortfalls, flag risk patterns and surface thought-provoking reflections, making sure care doesn’t stop at the counter. After a decade embedded in medical software development, we know the terrain. Fill up the form and let’s walk it together.

